
One of the most common diseases today isosteochondrosis of the lumbar spine. Both men and women equally often turn to doctors with this disease.
At least once in our lives, each of us has experienced pain in the lower back, sacrum or lower extremities. We often unconsciously call this type of pain "pinched nerve in the lower back. "
Causes of lumbar osteochondrosis
According to research conducted by doctors and scientists, the main cause of osteochondrosis of the lumbar spine is upright posture. However, not all people suffer from osteochondrosis. Provocative factors that accelerate the development of the disease are: metabolic disorders, physical inactivity, injuries, excess weight, improper weight lifting.
The source of pain in osteochondrosis is pinched nerve roots, which occur after protrusion of the intervertebral disc and narrowing of the intervertebral space. This deviation is formed when nutrition deteriorates, the natural processes of oxygen and lymph exchange in the tissues of the intervertebral discs are disrupted. As a result, the shock-absorbing capacity of the intervertebral discs decreases, and the nucleus pulposus of the disc gradually decreases and dries out.
From an anatomical point of view, lumbar osteochondrosis is a process of transformation of cartilage into bone, resulting in excessive pressure on the nerve roots extending from the spinal cord. This change causes pain. Overgrowth of bone tissue occurs due to deterioration of nutrition of the intervertebral discs, loss of fluid, and disturbances in structure and functioning.
When the protrusion of the intervertebral disc during the development of osteochondrosis of the lumbar spine becomes more severe, it causes the development of lumbar protrusion and lumbar disc herniation due to rupture of the fibrous ring.
Pain syndrome is formed due to pinching of the spinal nerve in lumbar osteochondrosis and is called lumboischialgia. This symptom is accompanied by numbness of the lower extremities. Depending on the nature and localization of pain, the disease can be divided into sciatica and low back pain. Inflammation of a nerve due to its pinching is called radiculitis. Methods of treating radiculitis with painkillers, in fact, are only the elimination of symptoms and are ineffective, because such treatment does not affect the real cause of the disease, namely degenerative processes in the intervertebral discs. To eliminate pain and take preventive measures to prevent complications, it is necessary to undergo a full course of treatment to activate the restoration processes in the tissues of the discs, normalize the height and physiological parameters of the intervertebral discs.
Symptoms of osteochondrosis of the lumbar spine

One of the signs of osteochondrosis is compression of the roots of the spinal nerves by the protruding nucleus pulposus of the intervertebral disc. This compression occurs in the epidural space, which is a sort of container for the spinal roots. Osteochondrosis of the lumbar spine manifests itself with the following symptoms which correspond to a compressed root:
- L1 and L2 – loss of sensation in the "rider's trousers" area, i. e. in the groin area and inner thigh. Pain can occur simultaneously in both legs if lumbar osteochondrosis is complicated by the development of a hernia.
- L5 – shooting pain, decreased sensation in the lower back and sensitivity of the thumb, as well as decreased ability to flex the finger.
- S1 – shooting pain, decreased sensation in the lower leg and outer thigh, pain in the foot from the little toe to the fourth toe. Often when this root is damaged, Achilles and plantar reflexes are lost.
- Damage to the Deproge-Gotteron artery: in the chronic course of osteochondrosis, paralysis of the lower leg and buttocks may occur, and sensitivity may disappear in the anogenital area.
- Simultaneous damage to the L5, S roots, and Deproge-Gotteron artery causes "paralyzing sciatica" syndrome, loss of pelvic and motor functions.
Osteochondrosis of the lumbar spine can cause protrusions and hernias due to significant loads on this part of the spine. It is these complications that develop very quickly, so it is very important to treat them in a timely manner. Do not delay the visit to a vertebrologist, undergo a comprehensive examination and seek qualified help at the first symptoms of lumbar osteochondrosis.
Complications of osteochondrosis of the lumbar spine
Vascular-compressive ischemia can be considered a complication of lumbar osteochondrosis. This pathology develops due to a reduced blood supply to the spinal cord, the reduction of intervertebral openings for vessels and arteries and the narrowing of the peripheral structures of the vertebrae. The reason for the development of this pathology is flattening of the discs, excessive mobility of the spine, weakened ligaments, the formation of osteophytes and neoatrosis. Permanent injury and pressure on a pinched vessel or artery occurs due to any movement of the spine affecting the damaged area. In addition, a reflex narrowing of the vessel passing through the blocked opening of the canal may develop. This effect is called "narrow bed".
Vertebrologists identify another serious complication of osteochondrosis of the lumbar spine. Compressive myelopathy is a spinal cord disease that occurs due to narrowing of the spinal canal. Depending on the location, the symptoms and severity of the condition may vary. Most often, the course of the disease is characterized by episodic nature: after the attack there is a period of remission.
Lumbar osteochondrosis can be complicated by a TXII-L1 herniated disc, which puts pressure on and causes damage to the S1-S2, L2-L-4 segments of the spinal cord. A patient with this complication experiences pain in the lower back, lower leg, back of the thigh, and weakness in the legs. The gluteal and calf muscles gradually become hypotonic and hypotrophic, Achilles and plantar reflexes decrease, and foot paresis forms. The posterior and external surfaces of the foot and lower leg are characterized by reduced sensitivity or its complete absence.
If a herniated disk LI-II develops, in which excessive pressure on the S3 coccygeal segment increases, osteochondrosis of the lumbar spine has the following symptoms: disruption of the pelvic organs, fecal and urinary incontinence, constipation, loss or decrease in sensitivity of the disc anogenital area, development of bedsores, anal prolapse reflex.
"Cauda equina syndrome" develops when the nerve roots are compressed from the first lumbar vertebra onwards. An experienced vertebrologist notes that this syndrome develops more often in patients with congenital narrowness of the spinal canal. The "cauda equina" is a bundle of nerve roots that contains the terminal roots of the spinal cord from the first segment onwards. The name comes from its resemblance to a horse's tail. The diagnosis of this syndrome largely depends on the presence of excruciating pain of a radicular nature. It is this feature that distinguishes cauda equina syndrome from other complications in which acute pain is not present.
Cauda equina syndrome is characterized by intense pain in the sacrum and lower back, radiating to the buttock, anogenital region, and posterior surface of the thigh. In some cases, paresis, peripheral paralysis and sensory disturbances occur. Severe cases are characterized by paralysis of the buttocks and both legs. A feature of the complication can be considered the asymmetry of sensory and motor disorders.
Lumbar osteochondrosis can cause the development of the myeloid syndrome of "intermittent claudication, " in which there is weakness in the legs while walking, frequent need to urinate, and numbness in the lower torso. The cause of this discomfort is poor blood supply to the lower parts of the spinal cord. After rest, these sensations disappear.
With ischemia of the roots of the cauda equina, caudogenic "intermittent claudication" occurs: goosebumps and tingling sensations when walking. Over time, this symptom may increase, reaching the perineum, genitals and groin. The weakness in the legs disappears after a short rest.
Compression of the Adamkiewicz artery can occur due to sudden unsuccessful movements, heavy lifting, or tremors. This complication of osteochondrosis of the lumbar spine manifests itself as disorders of the pelvic organs, loss of sensitivity, the appearance of bedsores and atrophy of the leg muscles.
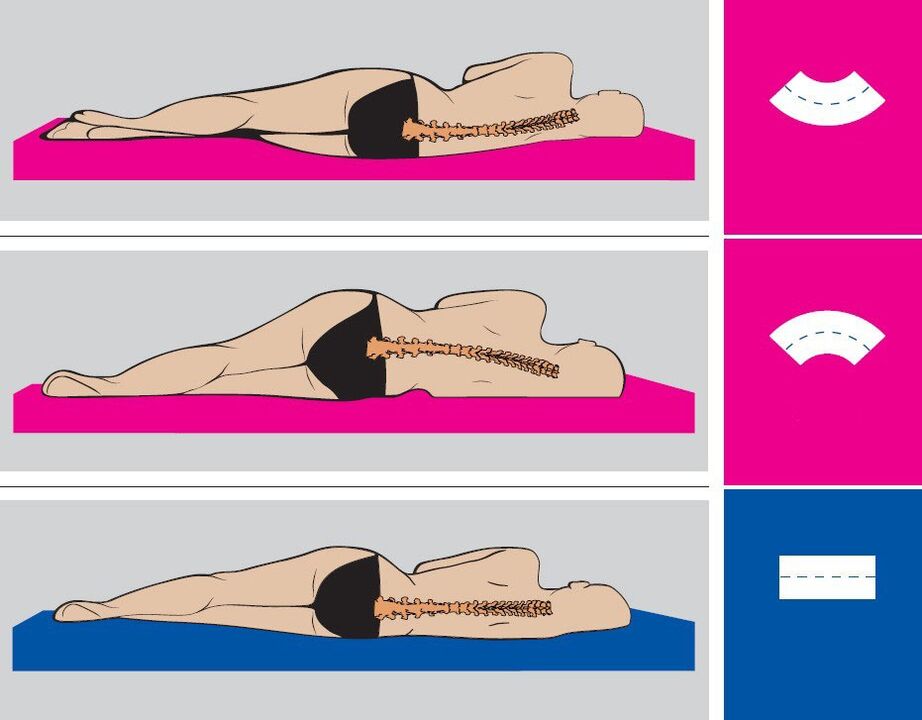
Osteochondrosis of the lumbar spine is manifested by aching pain in the lower back. Due to prolonged stay in an uncomfortable position, the pain may intensify. After sleeping or resting in the supine position, the pain decreases or disappears completely.
The occurrence of stressful situations for the body can cause the development of an acute condition. Most often this happens during hypothermia, heavy loads and sudden movements. A flare-up is characterized by severe pain, which can travel from the lower back to the legs. The body can independently try to reduce the load on the affected part of the spine by means of strong tension in the lumbar muscles. A patient with osteochondrosis of the lumbar spine tries to find a comfortable position in which the pain decreases.
Diagnosis of lumbar osteochondrosis
The diagnosis of osteochondrosis is carried out in several stages. The doctor needs to talk to the patient, ask about complaints, find out the nature of the pain, where it is localized, what time the painful sensations appear, their duration, intensity, etc. Also, the doctor will find out under what conditions the pain appears, when it intensifies or subsides.
Next, the vertebrologist examines the anamnesis, e. g. history of the disease. The doctor will certainly clarify how long the painful condition lasts, what was the cause of the pain and how you feel during the period when the discomfort disappears. An important point is preliminary treatment, as well as the effectiveness of certain treatment methods. A qualified doctor will certainly ask the patient about living and working conditions, freedom of movement, well-being under certain loads and past illnesses. It is very important to find out whether the patient has had spinal injuries, whether she has played sports and whether any close relatives have had spinal diseases.
The next step in diagnosis will be examining the patient. The doctor will pay attention to the position of the head, legs and arms in relation to the body, the gait, the way of holding oneself, the symmetry of the body areas, the condition of the skin in the damaged area and the patient's movements. Next, the range of motion of the spine and the level of damage are established. To do this, the doctor will ask the patient to bend forward, sideways, backwards, move different parts of the back and tilt the head. A healthy person should not feel any creaking or joint pain during such a simple test.
If the patient does not suffer from osteochondrosis, he can reach the chest and shoulder with his chin. Head movements in each direction are approximately 60 degrees. A 45 degree angle is formed by bending laterally between the head and the upper cervical spine. The distance from the sacrum to the spinous process of the seventh cervical vertebra increases by 5-7 centimeters when bending forward. This distance is reduced by 5-6 cm when you bend backwards. An experienced vertebrologist will pay attention to how the knee and hip joints participate in flexion and how the configuration of the spine changes.
Treatment of osteochondrosis of the lumbar spine
Lumbar osteochondrosis requires complex, intensive and long-term treatment. This is especially true for chronic cases with multiple intervertebral hernias and protrusions.
Effectivetreatment of osteochondrosis of the lumbar spineit is achieved with reflex methods that do not cause side effects, but bring maximum benefit. Remember, recovery from such a serious illness cannot come quickly. In each case of lumbar osteochondrosis, the doctor prescribes an individual treatment regimen.

It is worth noting that manual therapy can be used only in cases where the patient's spine is not damaged by intervertebral protrusions and hernias. The integrated use of these techniques allows you to restore normal blood microcirculation, eliminate congestion, vascular edema, relieve muscle spasms, restore the balance of metabolic processes in the tissues of the vertebrae and intervertebral discs, and also improve the nutrition of tissues in the lumbar region. As a result, the natural regeneration process is stimulated. It is worth noting that in case of lumbar osteochondrosis, manual therapy should be aimed at improving the functions of the spine.
Treatment procedures for lumbar osteochondrosis are complemented by the use of herbal remedies that improve the innervation of the body and also restore the balance of metabolic processes. The vertebrologist will advise patients on nutritional correction and a more active lifestyle. It is important to regulate body weight, because excess weight puts additional pressure on the lower back and also aggravates the development of osteochondrosis of the lumbar spine.
An experienced specialist treating osteochondrosis allows the patient to achieve serious results, as well as avoid surgery, improve motor activity, eliminate lower back pain and comprehensively improve the body to prevent further exacerbations. Acute pain disappears after 1-3 sessions of manual therapy, and the positive effect of treatment is achieved on average after 10-15 sessions. Remember that timely start of treatment is a guarantee of achieving positive results.
During the period of exacerbation of pain in the lower back, the patient is advised to stay in bed for 2-3 days. To quickly relieve pain, nonsteroidal anti-inflammatory drugs, painkillers, venotonics, diuretics, nicotinic acid and B vitamins are prescribed. To unload the spine, walking with crutches, dry or underwater traction of the spine may also be prescribed . If necessary, blocks with glucocorticoids or paravertebral blocks with anesthetic are prescribed.
Physiotherapy treatment of osteochondrosis of the lumbar spine may also include electrophoresis, laser therapy and ultraviolet radiation. Physical therapy is a mandatory component of a comprehensive treatment program. Some exercises can be used in the acute phase, but almost all exercises are recommended to be performed after the pain has subsided. Thanks to regular physical exercise, the nutrition of the tissues is restored, the blood and lymph supply to the intervertebral discs is improved and the flexibility and elasticity of the joints and cartilage are gradually restored. Thus, the patient's condition improves, and the interval between periods of exacerbation lengthens.
Spa treatments also have a good effect on health. In climatic resorts, iodine-bromine, hydrogen sulfide and radon baths are prescribed.
Surgical treatment methods are used only if the patient's pain cannot be relieved for a long time by conservative methods, with paresis of the muscles of the lower extremities and disruption of the processes of natural urination and defecation. During the surgery, the herniated disc is removed and the spinal segment is strengthened.
Prevention of lumbar osteochondrosis
Prevention of lumbar osteochondrosis consists in following simple rules recommended by a vertebrologist. He reminds that the development of the disease can be prevented only by carefully following these rules, no matter what:
- Keep your lower back dry and warm, do not overcool your spine and avoid drafts.
- Do not lift heavy objects or carry them long distances.
- Try not to make sudden movements.
- Maintain correct posture during work and rest.
- Change position as often as possible, trying not to stay in the same position for a long time.
- Do physical therapy.
- Try not to stay in a bent position for a long time.
- When cleaning, use a long brush, a broom, and a vacuum cleaner with a long hose so you don't have to bend over.
- Lift weights correctly: bend over with a straight back, or bend your knees, pick up the bags with a straight back and stand up straight. Keep your hands with the load as close to your body as possible.
- If you need to bend down to pick something up off the floor, such as under the table or bed, get down on one knee and keep your back straight.
- Distribute the weights equally between two hands.
- Strengthen your gluteal muscles, lengthen your spine, take a walk every day.
- Balance your diet, enrich your diet with dairy products and plant products.
- Stick to the drinking regime: 1. 5-2 liters of water and herbal teas per day.
- Get rid of bad habits: alcohol, smoking, drugs.



















